Birth control is crucial for reproductive health, empowering individuals in family planning.
Yet, myths persist, causing confusion!
Let’s debunk these myths about birth control for informed decisions.
Here are the 5 Common Myths About Birth Control:
- You Will Gain Weight on Birth Control
- Contraceptives Cause Infertility
- Birth Control is 100% Effective
- Decreases Libido on Birth Control
- Only Young Women Need Birth Control
[toc]

Myth 1: Birth Control is a Scam
Why This Myth Exists:
The notion that birth control is a scam may stem from various sources, including misinformation, societal stigma, or personal anecdotes.
Some individuals might have suspicions due to the historical context of reproductive health, where misinformation or lack of understanding prevailed.
Debunking the Myth:
Birth control, specifically hormonal contraceptives like birth control pills, patches, and injections, is not a scam.
These methods are designed to regulate hormonal levels to prevent ovulation, and fertilization, or alter the uterine lining to inhibit implantation.
Birth control provides individuals with a choice in family planning and offers various health benefits, such as managing menstrual irregularities, reducing menstrual cramps, and improving acne.
Myth 2: You Will Gain Weight on Birth Control
Why This Myth Exists:
One reason people believe that birth control causes weight gain is because of changes in hormones and weight that happen naturally during a woman’s menstrual cycle.
Sometimes, individuals mix up these changes and think they’re caused by birth control.
Also, stories about possible side effects, like gaining weight, get shared among friends and family, making people worried about it.
Debunking the Myth:
Scientific studies generally do not support a significant link between birth control and weight gain.
While some people may experience minor fluctuations, it’s essential to recognize that various factors contribute to weight changes, including lifestyle, diet, and genetics.
Birth control methods come in various formulations, and each person’s response can be unique.
It’s crucial to consult with a healthcare professional to find a method that suits individual health needs and concerns.
Myth 3: Contraceptives Cause Infertility
Why This Myth Exists:
When individuals decide to discontinue contraceptive methods to conceive, there might be a delay in achieving pregnancy.
This delay is a normal aspect of the body readjusting to its natural hormonal balance.
Unfortunately, this natural process is sometimes misunderstood, leading to the false belief that contraceptives have caused infertility.
Debunking the Myth:
Birth control methods are designed to be reversible, and fertility typically returns after discontinuation.
Contraceptives prevent pregnancy by inhibiting ovulation, thickening cervical mucus, or altering the uterine lining.
Once these methods are stopped, the body generally returns to its natural reproductive function. There is no evidence to support the claim that birth control leads to permanent infertility.
Myth 4: You Can’t Get Pregnant While on Your Period
Why This Myth Exists:
This myth suggests that pregnancy is impossible during menstruation due to a combination of factors, often stemming from misunderstandings about the menstrual cycle and fertility.
Misunderstandings about fertility awareness and the complexities of the reproductive system during different phases of the menstrual cycle further contribute to the belief that pregnancy is improbable during menstruation.
A general lack of comprehensive education about the complexities of the reproductive system may fuel this belief.
Debunking the Myth:
Menstrual cycles can vary in length among different individuals, and even in the same person from one cycle to the next.
While some women have regular 28-day cycles, others may have shorter or longer cycles.
This variability can affect the timing of ovulation, making it possible for conception to occur shortly after menstruation ends.
Sperm can survive in the female reproductive tract for several days.
If a woman has a shorter menstrual cycle and ovulates shortly after her period, sperm deposited during menstruation may still be viable when ovulation occurs, leading to a potential risk of pregnancy.
Myth 5: You Will Get STI Protection on Birth Control
Why This Myth Exists:
One key reason for this myth is the confusion between various forms of contraception.
While some methods, such as condoms, provide a degree of protection against STIs, hormonal birth control methods like pills, patches, or injections primarily focus on preventing pregnancy by inhibiting ovulation or affecting the uterine lining.
The lack of distinction between these different types of contraceptives can contribute to the view that all birth control methods offer STI protection.
Debunking the Myth:
Most birth control methods focus on preventing pregnancy and do not offer protection against STIs. Condoms, on the other hand, are effective in reducing the risk of most STIs.
In the same way, dual protection involves using both hormonal birth control and barrier methods, such as condoms, to simultaneously prevent pregnancy and protect against STIs.
These methods, when used with precision, are effective in preventing STIs. Otherwise, it’s not the case that simply being on a birth control pill will help you be safe from STIs.
Myth 6: Birth Control is 100% Effective
Why This Myth Exists:
The notion that birth control is infallible might stem from a desire for absolute certainty in family planning.
People seeking reliable contraceptive methods might assume that if a particular birth control method is adhered to correctly, it should guarantee complete protection against unintended pregnancies.
Debunking the Myth:
No contraceptive method is 100% foolproof. Even with perfect use, there is always a small risk of pregnancy.
Effectiveness rates are based on averages and may vary among individuals.
It’s crucial for users to be aware of the specific efficacy of their chosen method and consider additional precautions when necessary.
Myth 7: You Can’t Get Pregnant if You Miss One Pill
Why This Myth Exists:
Users might not receive explicit instructions on what to do in the event of a missed dose or may not fully understand the time-sensitive nature of contraceptive effectiveness.
So it is unclear or insufficient communication about the consequences of missing a pill that can lead to such misconceptions.
Debunking the Myth:
Missing a pill, especially during a critical part of the menstrual cycle, can potentially disrupt the hormonal balance necessary for contraception, increasing the risk of ovulation and, consequently, pregnancy.
Therefore, it’s essential to follow healthcare provider instructions meticulously and consider backup methods, such as condoms, when a pill is missed.
Myth 8: Depo Birth Control Shot Leads to Cervical Cancer
Why This Myth Exists:
Some individuals may lack a comprehensive understanding of cervical cancer causes, leading them to attribute the condition to specific contraceptive methods.
Likewise, Fear and mistrust of contraceptives, especially hormonal methods, can lead to the acceptance of unfounded claims
Debunking the Myth:
The claim that the Depo shot causes cervical cancer is not supported by scientific evidence.
The Depo-Provera shot is a progestin-only contraceptive method that works by suppressing ovulation, thickening cervical mucus, and altering the uterine lining.
Cervical cancer, on the other hand, is predominantly caused by persistent infection with certain strains of the human papillomavirus (HPV).
The idea may stem from a misunderstanding of correlation versus causation.
While some studies have explored the relationship between hormonal contraceptives and HPV infection, the consensus is that the use of hormonal birth control does not directly cause cervical cancer.
It is crucial to highlight that regular cervical screenings (Pap smears) and the HPV vaccine are more effective strategies for preventing cervical cancer.
These measures address the root cause—HPV infection—rather than attributing cancer risk to a specific birth control method.
Myth 9: You Should Take a Break from Birth Control
Why This Myth Exists:
Historically, there have been concerns about potential long-term effects or uncertainties about the continuous use of contraceptives.
Additionally, cultural or societal narratives may have contributed to the misconception that periodic breaks are necessary for overall health or fertility.
Debunking the Myth:
Continuous use of birth control is generally safe and can offer health benefits, such as reduced menstrual pain and improved skin conditions.
There is no medical necessity for taking breaks, and doing so may increase the risk of unintended pregnancies.
Myth 10: Only Women Need to Worry About Birth Control
Why This Myth Exists:
Traditional gender roles and historical societal expectations often place the responsibility of contraception solely on women.
In many cultures, women have been assigned the primary role of managing family planning, reinforcing the misconception that birth control is exclusively their concern.
Additionally, limited historical contraceptive options for men may have contributed to this perception.
Debunking the Myth:
Both men and women share responsibility for family planning, and various contraceptive methods are available for men to actively participate in preventing unplanned pregnancies.
Couples should engage in open communication about family planning goals, and both partners should actively participate in choosing a contraceptive method that aligns with their preferences and lifestyles.
Myth 11: The Pill Protects Against HIV
Why This Myth Exists:
This view likely arises from confusion between the prevention of pregnancy and protection against sexually transmitted infections (STIs) like HIV.
Some individuals might assume that because birth control methods involve intimate aspects of sexual health, they provide a comprehensive shield against various risks, including HIV.
Debunking the Myth:
Birth control pills are designed to prevent pregnancy by regulating hormones, but they do not offer any defense against sexually transmitted infections.
As already discussed in the above section, condoms are the most effective method for protecting against HIV and other STIs as they create a barrier preventing the exchange of bodily fluids.
Combining condom use with other contraceptive methods provides a holistic approach to sexual health.
Myth 12: Birth Control Causes Mood Swings
Why This Myth Exists:
Media portrayals and personal stories, although valuable, may amplify individual experiences, leading to a generalization that birth control universally induces mood swings.
The complex interplay of hormones within the body, coupled with varied responses to contraceptive methods, contributes to the persistence of this myth.
Debunking the Myth:
While a small percentage of users may experience mood changes, scientific evidence does not consistently support a direct link between birth control and mood swings.
Factors such as stress, lifestyle, and underlying mental health conditions can influence mood.

Myth 13: Birth Control Pills Cause Abortions
Why This Myth Exists:
Some individuals may associate any interference with a fertilized egg as an abortion, irrespective of the medical definition.
Lack of clarity on the precise mechanisms of birth control contributes to the perpetuation of this myth.
Debunking the Myth:
Birth control pills primarily work by preventing ovulation, fertilization, or altering the uterine lining to inhibit implantation.
They are not intended or designed to induce abortions. If a woman is already pregnant, using birth control pills will not terminate the pregnancy.
It’s crucial to distinguish between contraceptive methods and medications designed for abortion.
Myth 14: The Morning-After Pill is the Same as an Abortion Pill
Why This Myth Exists:
The terms ‘morning-after pill’ and ‘abortion pill’ are sometimes used interchangeably or confused due to their relationship with stopping pregnancy.
This lack of clarity in terminology can lead to the notion that both pills serve the same purpose.
Debunking the Myth:
The morning-after pill primarily works by inhibiting ovulation or fertilization, preventing pregnancy before it occurs.
It is not the same as medications used for abortion, which are designed to terminate an established pregnancy.
Emergency contraception is a preventive measure, not a method for ending an existing pregnancy.
Myth 15: Antibiotics Reduce Birth Control Effectiveness
Why This Myth Exists:
Antibiotics are often associated with treating infections, and there is a belief that they might interfere with the effectiveness of hormonal contraceptives, such as birth control pills.
Additionally, historical information and some early studies suggested a potential interaction between certain antibiotics and hormonal contraceptives.
As a result, this idea became ingrained in popular belief, contributing to the persistence of the myth.
Debunking the Myth:
While some antibiotics may interact with certain hormonal contraceptives, the impact on effectiveness is often minimal.
The antibiotics that are commonly prescribed do not universally reduce the efficacy of birth control pills.
However, for individuals prescribed antibiotics and using hormonal birth control, it’s advisable to consult with healthcare providers or pharmacists to understand potential interactions and, if needed, consider additional contraceptive measures during antibiotic treatment.
Myth 16: Birth Control Targets Healthy Parts of the Body
Why This Myth Exists:
The complex hormonal mechanisms in various forms of birth control can be challenging for some individuals to fully grasp.
This limited understanding may contribute to the false belief that birth control targets healthy parts of the body.
Plus, when individuals notice changes in their menstrual cycle or experience side effects, they might mistakenly interpret these as the contraceptive targeting healthy aspects of the body, rather than understanding its intended impact on fertility.
Debunking the Myth:
Birth control is designed to regulate reproductive processes without causing harm to healthy body parts.
Hormonal contraceptives primarily target the reproductive system by influencing hormone levels, preventing ovulation, or altering the uterine environment.
These alterations are reversible, and the overall health benefits often outweigh the potential risks for many individuals.
It’s essential to understand that the hormonal changes induced by birth control are generally within the normal physiological range and contribute to effective contraception without causing harm to other vital systems.
Myth 17: Contraceptives Have More Cons Than Pros
Why This Myth Exists:
One possible contributing factor to this myth is the diversity of contraceptive methods available, each with its own set of benefits and side effects.
Individuals might perceive side effects, such as hormonal changes, mood swings, or physical discomfort, as significant cons.
Additionally, misinformation or lack of comprehensive education about contraceptives may contribute to an exaggerated perception of their drawbacks.
Debunking the Myth:
Assessing the pros and cons of contraceptives is a subjective process that varies among individuals. While some people may experience drawbacks, such as mild side effects, the benefits of contraceptives often outweigh the potential drawbacks.
Contraceptives offer effective family planning, regulate menstrual cycles, reduce the risk of certain cancers, and provide various health benefits.
The decision to use contraceptives should be based on individual health needs and preferences.
Labeling contraceptives as having universally more cons than pros oversimplifies the nuanced considerations involved in reproductive health decisions.
Myth 18: Decreases Libido on Birth Control
Why This Myth Exists:
Birth control methods, especially hormonal ones, can lead to fluctuations in hormone levels. Some individuals may experience changes in libido due to these hormonal shifts.
If individuals notice a decrease in sexual desire while on birth control, they might attribute it to the contraceptive method, creating the perception of a causal relationship.
Debunking the Myth:
While some individuals may experience changes in sexual desire, research does not consistently support a direct link between birth control and decreased libido for everyone.
Individual responses to hormonal changes vary, and it’s essential to communicate openly with healthcare providers about any concerns, as they can help explore alternative contraceptive options.
Myth 19: The Pull-Out Method is Very Ineffective
Why This Myth Exists:
The myth may stem from an underestimation of the risk associated with pre-ejaculation (pre-cum).
While the pull-out method relies on withdrawing before ejaculation, pre-ejaculation can contain sperm, leading to the misconception that this method is highly ineffective.
Debunking the Myth:
Contrary to the common perception, data indicates that the pull-out method can be more effective than often assumed.
The typical use effectiveness rate of 78% implies that, with regular use, approximately 22 out of 100 people may experience unintended pregnancies within a year.
While this rate is not as high as some other methods, it challenges the notion that the pull-out method is extremely unreliable.
Moreover, when used perfectly—meaning withdrawal is timed accurately and consistently—the effectiveness rate increases to 96%.
This places it in close proximity to the effectiveness of condoms (82% with typical use, 98% with perfect use).
While the pull-out method does not protect against sexually transmitted infections (STIs), its effectiveness in preventing pregnancy challenges the perception that it is inherently irresponsible.
Myth 20: Wearing Two Condoms (Double Bagging) Causes Condoms to Break
Why This Myth Exists:
The myth of wearing two condoms causing them to break likely originates from concerns about increased friction between the condoms.
The belief suggests that the rubbing of two layers of latex or polyurethane may compromise the structural integrity of both condoms, leading to a higher likelihood of breakage.
Debunking the Myth:
Scientific evidence challenges the assumption that double bagging leads to an increased risk of condom breakage.
The study’s findings suggest that double bagging does not necessarily compromise the integrity of condoms.
While it is generally recommended to use a single condom correctly and consistently, the idea that wearing two condoms is inherently problematic or increases the risk of breakage is not supported by empirical evidence.
Myth 21: You Need to Take Birth Control Pills at the Same Time Every Day
Why This Myth Exists:
Some individuals may generalize the importance of consistency in taking pills, and while this is crucial for certain types of birth control pills, the myth might emerge from a broad interpretation of the need for regularity.
Healthcare providers often stress the importance of establishing a daily routine for taking medications.
While this advice is valid for promoting adherence, the emphasis on a specific time might be interpreted more rigidly than intended, contributing to the myth
Debunking the Myth:
For combined pills, missing a dose can be compensated by taking the missed dose as soon as remembered and the next one at the regular time.
However, after the placebo week, consistency is crucial to maintain hormone levels and effectiveness.
Progestin-only pills require strict daily adherence due to concerns about interference with lactation.
Myth 22: Only Young Women Need Birth Control
Why This Myth Exists:
Media representations and advertising campaigns that predominantly feature younger individuals in the context of birth control can contribute to the myth.
If older women are not prominently depicted in discussions about contraception, it may reinforce the idea that birth control is exclusively for younger age groups.
Debunking the Myth:
Birth control methods are not age-restricted, and individuals of all ages, including those approaching menopause, may still need contraception if they are sexually active and not ready for pregnancy.
Choosing a suitable method should be based on health, lifestyle, and reproductive goals, regardless of age.
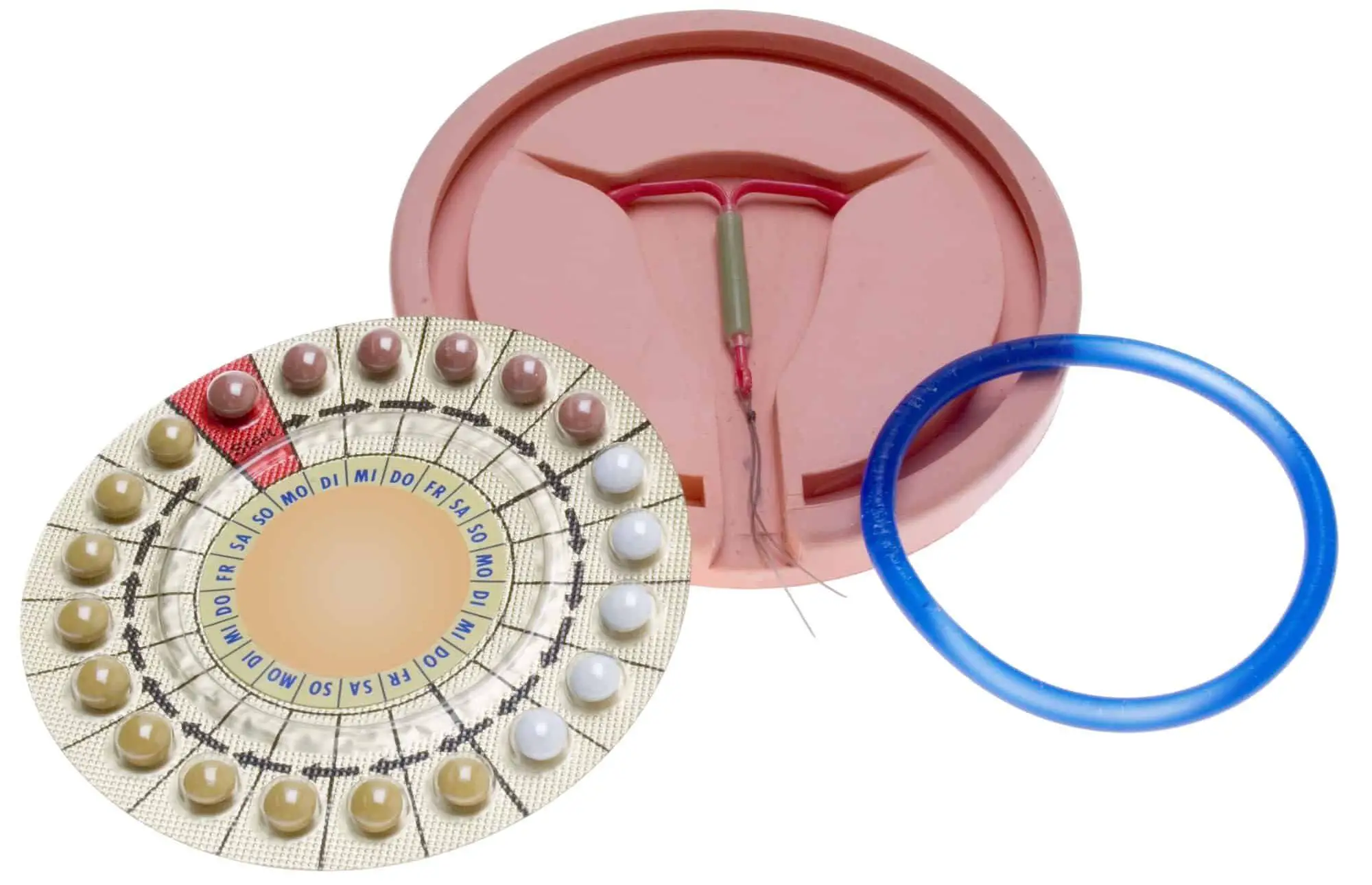
Myth 23: All Birth Control Methods are the Same
Why This Myth Exists:
People may assume that all methods function in a similar manner to prevent pregnancy.
The oversimplification of birth control options can stem from limited education on the subject, leading individuals to believe that one method fits all scenarios.
Debunking the Myth:
Different birth control methods operate through various mechanisms.
While hormonal methods, such as pills, patches, and injections, regulate hormones to prevent ovulation, barrier methods like condoms physically block sperm.
Intrauterine devices (IUDs) prevent fertilization in yet another way. Recognizing these distinctions dispels the notion of uniformity.
Birth Control Myths FAQs
What are some negative facts about birth control pills?
Birth control pills, while effective, can have potential side effects, including nausea, headaches, mood changes, and changes in libido. They may also increase the risk of blood clots in some individuals.
It’s essential to consult with a healthcare provider to discuss potential risks and benefits based on individual health.
How effective is birth control without pulling out?
The effectiveness of birth control without pulling out varies depending on the method used. For example, birth control pills, when taken correctly, are over 90% effective.
However, combining methods, such as using birth control pills along with condoms, can enhance overall effectiveness.
Can birth control affect climax?
Some individuals may experience changes in sexual desire or arousal while on birth control, but its impact on climax can vary. While some people report no noticeable effects, others may experience changes in orgasm intensity or frequency.
Individual responses to hormonal contraceptives differ, and it’s crucial to communicate any concerns with a healthcare provider.
Is birth control a real thing?
Yes, birth control is a real and widely used method to prevent unplanned pregnancies. It includes various contraceptive options such as birth control pills, patches, injections, intrauterine devices (IUDs), and more.
Is birth control 100% protection?
No, birth control is not 100% foolproof. While many methods are highly effective when used correctly, there is always a small chance of failure.
Consistent and proper use significantly reduces the risk of pregnancy, but it does not provide absolute protection.
How proven is birth control?
Birth control methods undergo extensive testing and research to ensure their safety and efficacy.
Many methods, such as birth control pills and IUDs, have a high level of scientific evidence supporting their effectiveness when used as directed.
Can I trust my birth control?
Trust in birth control depends on its type and proper use. When used consistently and correctly, most methods are reliable. However, factors like forgetting to take pills or missing appointments for injections can affect their effectiveness.
Open communication with a healthcare provider is crucial to ensure the chosen method aligns with individual needs and lifestyles.
Is birth control safer than condoms?
Safety depends on individual circumstances and preferences. Condoms not only provide contraceptive protection but also offer a barrier against sexually transmitted infections (STIs).
Birth control methods like pills or IUDs focus primarily on preventing pregnancy. The choice between them often involves considering both contraceptive needs and STI prevention.
Is every girl on birth control?
No, not every girl is on birth control. Contraceptive choices vary among individuals based on personal preferences, health considerations, and lifestyle.
Some girls may choose not to use birth control, while others may opt for different methods.
Which contraceptive is best for unmarried girls?
The best contraceptive for unmarried girls depends on individual preferences, health considerations, and lifestyle. Common options include birth control pills, condoms, IUDs, and implants.
It’s essential to consult with a healthcare provider to determine the most suitable method based on individual needs.
What are the 5 methods of birth control?
The five common methods of birth control include:
- Birth control pills
- Condoms
- Intrauterine Devices (IUDs)
- Birth control patches
- Birth control injections
Are female condoms safer?
Female condoms are a safe and effective method of contraception. They provide a barrier against both pregnancy and STIs. However, their effectiveness depends on correct and consistent use.
As with any contraceptive method, proper education and understanding of use are crucial for optimal safety.