Communication is central to nursing practice, shaping how nurses engage with patients, exchange information, and collaborate with healthcare teams.
In nursing, communication is more than just words; it’s about establishing trust and ensuring patients feel heard and supported.
This article will discuss the importance of communication in nursing.
Additionally, we’ll offer practical tips for nurses to refine their communication skills, promoting better outcomes and nurturing a culture of compassionate care.
[toc]
9 Reasons Why Communication In Nursing Matters
Below, you’ll find a list of nine reasons emphasizing the significance of effective communication in nursing.

1. Preventing Medical Errors
Employing clear and effective communication techniques is vital to prevent medical errors.
When healthcare providers communicate clearly with each other and with patients, it ensures that everyone is on the same page regarding treatment plans, medication administration, and other important aspects of care.
This reduces the likelihood of mistakes or misunderstandings that could lead to adverse events.
For example, using simple language and visual aids can help improve patients’ medical education, allowing them to better understand their treatment instructions and reducing the risk of medication errors.
2. Building Trust
Establishing trust with patients through consistent and empathetic communication is essential for promoting a positive patient-provider relationship.
When patients feel listened to, respected, and understood, they are more likely to trust their healthcare providers and actively participate in their care.
Taking the time to explain procedures, answer questions, and address concerns helps to build this trust.
Additionally, maintaining a friendly and approachable demeanor can help patients feel more comfortable discussing their health concerns openly.
3. Enhancing Teamwork and Coordination
Effective communication strategies are key for seamless teamwork and collaboration among healthcare professionals.
When everyone involved in a patient’s care communicates clearly and regularly, it improves coordination and reduces the risk of errors.
For example, using tools like handoff reports and huddles can ensure that important information is shared between shifts and across disciplines.
This helps to ensure that all members of the healthcare team are working together toward the same goals and providing consistent, high-quality care.
4. Ensuring Smooth Care Transitions
Prioritizing accurate communication during care transitions is crucial to ensure the seamless transfer of patient information.
When patients move between different healthcare settings or providers, it’s essential that relevant information is communicated accurately and promptly to minimize gaps in care and prevent errors.
This might include ensuring that discharge instructions are clear and easy to understand and that patients know who to contact if they have questions or concerns after leaving the hospital.
5. Promoting Cultural Sensitivity
Demonstrating sensitivity and respect in communication with patients from diverse backgrounds is essential for providing equitable and culturally competent care.
This means being aware of and respectful of patients’ cultural beliefs, values, and practices, and adapting communication styles accordingly.
For example, using interpreters or translators when necessary can help ensure that language barriers don’t impede communication.
Additionally, taking the time to learn about patients’ cultural backgrounds and preferences can help healthcare providers deliver more personalized and effective care.
6. Empowering Patients Through Education
Providing clear and comprehensive instructions to patients regarding their treatment plans, medications, and self-care practices empowers them to actively participate in their healthcare decisions.
When patients understand their conditions and treatment options, they are better equipped to make informed choices and manage their health effectively.
This might involve using visual aids, written materials, or multimedia resources to supplement verbal instructions and ensure that patients have the information they need to take control of their health.
7. Upholding Ethical Standards
Maintaining transparent and ethical communication with patients is essential for upholding professional standards of practice.
This means providing patients with honest and accurate information about their diagnoses, treatment options, and prognosis, and respecting their right to make informed decisions about their care.
Additionally, it involves obtaining informed consent for treatments and procedures, and ensuring that patients understand their rights and responsibilities as healthcare consumers.
8. Driving Quality Improvement
Utilizing communication channels to gather feedback, share best practices, and address communication barriers is essential for driving continuous improvement in patient care delivery.
This might involve soliciting input from patients and staff about their experiences identifying areas for improvement, and implementing strategies to address these issues.
For example, conducting regular patient satisfaction surveys can help identify areas where communication could be improved, and implementing staff training programs can help address skill gaps and improve communication effectiveness.
9. Enhancing Patient Satisfaction
Prioritizing positive communication experiences is essential for enhancing patient satisfaction.
When patients feel valued, respected, and involved in their care, they are more likely to have positive experiences and outcomes.
This might involve taking the time to listen to patients’ concerns, addressing their questions and preferences, and involving them in decision-making about their care.
Additionally, maintaining open lines of communication and providing opportunities for feedback can help ensure that patients feel heard and supported throughout their healthcare journey.
15 Practical Tips for Enhancing Communication in Nursing
After learning how important communication is in nursing, if you want to get better at it, here are 15 simple tips for you.
They’ll help you connect better with patients and colleagues, making the care you give even better.
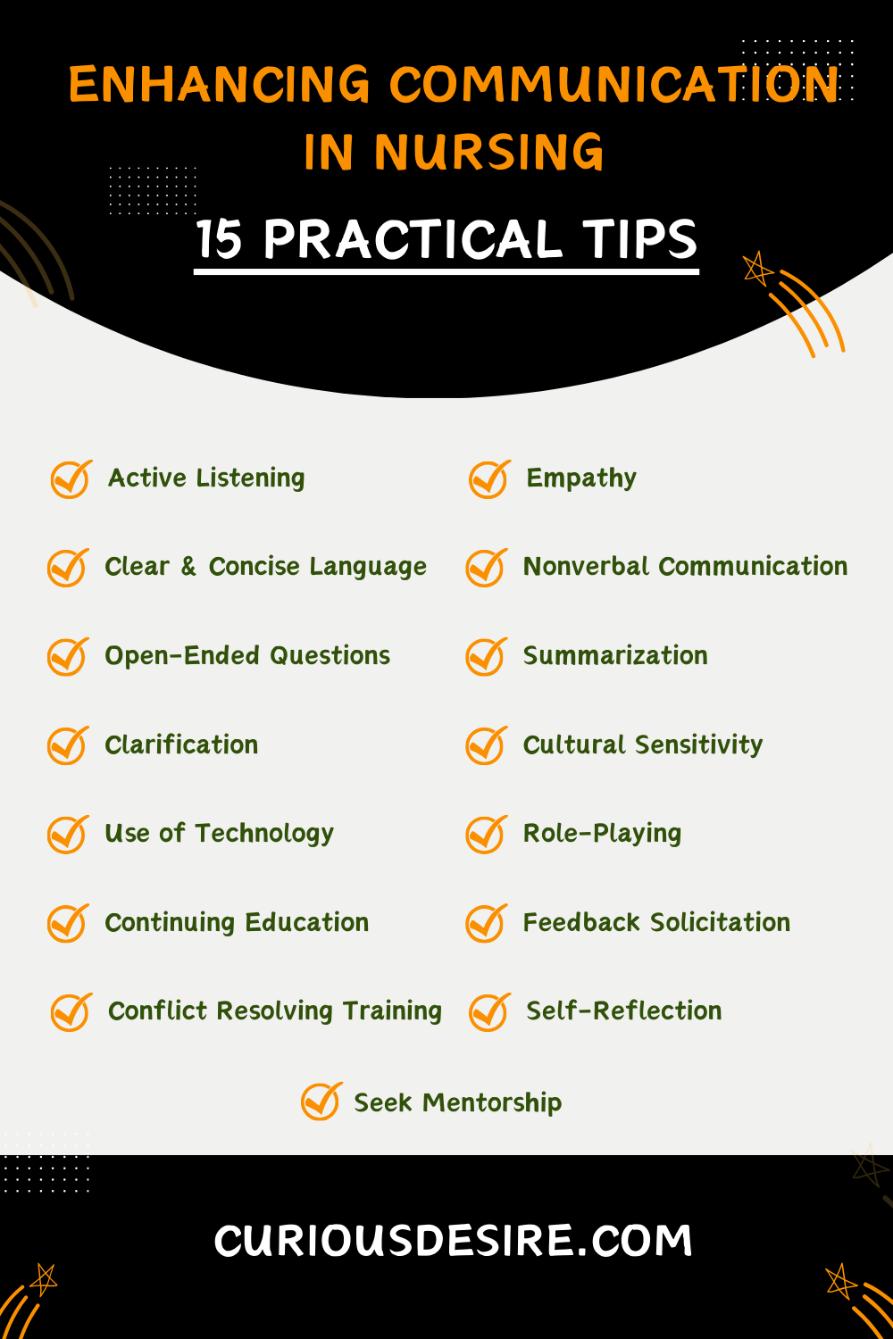
1. Active Listening
Active listening is a foundational skill for effective communication in nursing.
It involves giving your full attention to the patient, maintaining eye contact, and using verbal and non-verbal cues to show that you are engaged in the conversation.
Active listening also includes reflecting on what the patient has said to ensure understanding and convey empathy.
By actively listening to patients, nurses can build trust, establish rapport, and better address their needs and concerns.
2. Empathy
Empathy is a crucial component of patient-centered care and involves understanding and acknowledging the emotions and experiences of the patient.
Nurses can demonstrate empathy by actively listening, validating the patient’s feelings, and expressing compassion.
Using phrases such as “I understand how you feel” or “That must be difficult for you” can help convey empathy and support.
By showing empathy, nurses can strengthen their relationships with patients, enhance patient satisfaction, and contribute to improved health outcomes.
3. Clear and Concise Language
Clear and concise communication is essential for ensuring that patients understand the information provided to them.
Nurses should use simple language and avoid medical jargon or complex explanations.
Breaking down information into smaller chunks and providing explanations in a step-by-step manner can help patients grasp the information more easily.
Encouraging patients to ask questions and seeking feedback to ensure understanding are also important aspects of clear communication.
4. Nonverbal Communication
Nonverbal communication, including body language, facial expressions, and gestures, plays a significant role in conveying messages and building rapport with patients.
Nurses should be mindful of their body language, maintain an open and approachable posture, and use appropriate facial expressions to convey empathy and support.
Nonverbal cues such as nodding or leaning slightly forward can also indicate attentiveness and engagement in the conversation.

5. Open-Ended Questions
Open-ended questions encourage patients to share more information and provide insights into their thoughts and feelings.
Nurses should use open-ended questions that prompt patients to elaborate on their experiences and concerns.
For instance, nurses can ask “Can you tell me more about how you’re feeling?” or “What has been your experience with this condition?”
By asking open-ended questions, nurses can gather valuable information, promote patient-centered care, and establish trust and collaboration.
6. Summarization
Summarizing key points during conversations with patients helps ensure mutual understanding and clarifies any misunderstandings.
Nurses can summarize what the patient has said by paraphrasing their statements and highlighting important information.
Summarization can also serve as a checkpoint to verify accuracy and reinforce key takeaways from the conversation.
By summarizing effectively, nurses can enhance communication, address patient concerns, and promote shared decision-making.
7. Clarification
Clarification is essential for ensuring that both parties in a conversation understand each other correctly.
Nurses should not hesitate to ask for clarification if they are unsure about something a patient has said.
Using phrases such as “Could you please explain that to me again?” or “I want to make sure I understand correctly…” can help clarify any misunderstandings and ensure accurate communication.
By seeking clarification, nurses can demonstrate their commitment to understanding the patient’s needs and concerns fully.
8. Cultural Sensitivity
Cultural sensitivity is crucial for effective communication with patients from diverse backgrounds.
Nurses should be mindful of cultural differences in communication styles, gestures, and norms and adapt their approach accordingly.
Respecting patients’ cultural beliefs and preferences builds trust, enhances patient satisfaction, and promotes equitable and culturally competent care delivery.
Nurses can demonstrate cultural sensitivity by listening actively, acknowledging cultural differences, and being open to learning about and respecting patients’ cultural backgrounds.
9. Use of Technology
Utilizing technology tools and platforms can enhance communication and information sharing in healthcare settings.
Nurses should familiarize themselves with electronic health records (EHRs), medical apps, and telehealth platforms to streamline communication with patients and colleagues.
Technology can facilitate remote consultations, secure messaging, and access to patient information, improving efficiency and coordination of care.
By embracing technology, nurses can enhance communication, facilitate patient engagement, and improve the overall quality of care.
10. Role-Playing
Engaging in role-playing exercises allows nurses to practice communication skills in various scenarios and receive feedback from colleagues or mentors.
Role-playing helps nurses develop confidence, refine their communication techniques, and learn how to handle difficult conversations or address sensitive topics effectively.
By simulating real-life scenarios in a safe and supportive environment, role-playing enhances nurses’ communication skills and prepares them to navigate challenging situations confidently and professionally.
11. Continuing Education
Continuing education programs, workshops, and online courses provide valuable opportunities for nurses to enhance their communication skills and stay updated on best practices.
Nurses can participate in communication-focused training sessions to learn new techniques, strategies, and approaches for effective communication in healthcare settings.
12. Feedback Solicitation
Actively seeking feedback from patients, colleagues, or supervisors is essential for nurses to assess their communication skills and identify areas for improvement.
Nurses can ask for feedback on their communication style, listening skills, and patient interactions to gain valuable insights and perspectives.
Constructive feedback enables nurses to refine their communication techniques, address any communication barriers, and enhance the quality of their patient care.
By soliciting feedback, nurses demonstrate their commitment to continuous improvement and professional development.
13. Conflict Resolution Training
Conflict resolution training equips nurses with the skills and strategies needed to effectively manage conflicts and resolve disagreements in healthcare settings.
Nurses learn techniques for de-escalating tense situations, active listening, and finding mutually agreeable solutions to conflicts.
Conflict resolution training enhances nurses’ communication skills, promotes collaboration and teamwork, and provides a positive work environment conducive to quality patient care.
By developing proficiency in conflict resolution, nurses can navigate challenging situations with confidence, professionalism, and respect for all parties involved.
14. Self-Reflection
Self-reflection is a valuable practice that allows nurses to evaluate their communication interactions, identify strengths and areas for improvement, and set goals for professional growth.
Nurses can reflect on their communication experiences with patients, colleagues, and other healthcare professionals, considering what went well and what could have been done differently.
Self-reflection promotes self-awareness, enhances critical thinking skills, and encourages continuous learning and development.
By engaging in regular self-reflection, nurses can refine their communication skills, build confidence, and strive for excellence in patient care delivery.
15. Seek Mentorship
Seeking mentorship from experienced nurses or communication experts provides valuable guidance, support, and feedback on communication skills development.
Nurses can benefit from the knowledge, insights, and expertise of mentors who can offer personalized advice and encouragement.
Mentorship relationships facilitate professional growth, promote self-confidence, and enhance communication competence.
By seeking mentorship, nurses can accelerate their learning, gain valuable perspectives, and become more effective communicators in their nursing practice.
Importance Of Communication In Nursing – FAQs
1. Why is communication so important in nursing?
Communication in nursing is vital for patient care, safety, and outcomes. It helps nurses build rapport, understand patient needs, and collaborate effectively with healthcare teams.
Clear communication prevents errors, enhances satisfaction, and fosters trust, leading to better health outcomes.
2. How is communication used in the nursing process?
Communication is integral to every step of the nursing process. Nurses use it to gather information during assessments, collaborate on care plans, implement interventions, and evaluate patient progress.
Effective communication ensures accurate documentation, coordination of care activities, and informed decision-making.
3. What is the importance of communication in nursing informatics?
In nursing informatics, communication is essential for integrating nursing science with technology. Clear communication facilitates accurate documentation and sharing of patient information across electronic health records and telehealth platforms.
It enables real-time data access, remote collaboration, and informed clinical decisions, ultimately enhancing nursing practice and patient outcomes in the digital era.