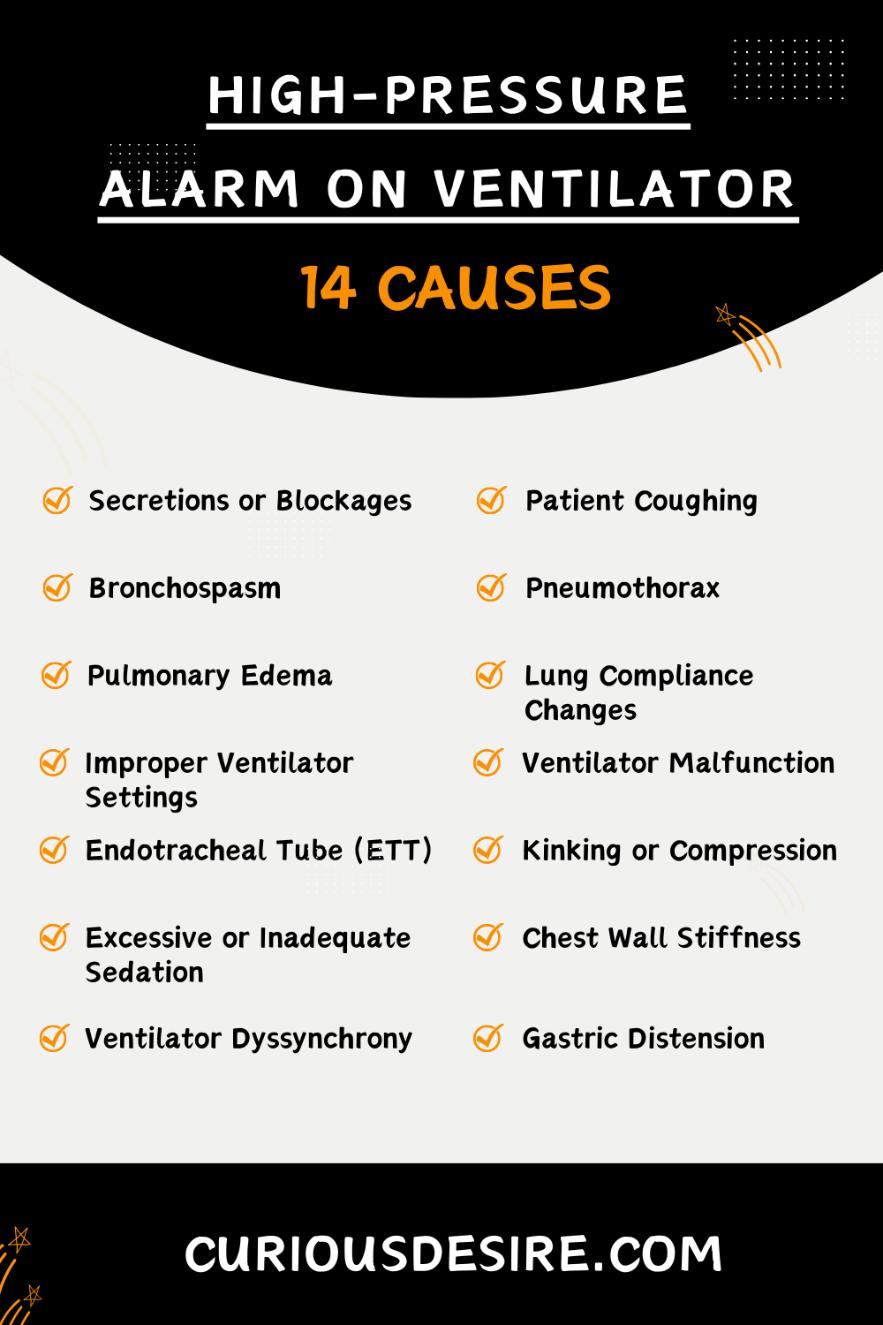
High-pressure alarms on ventilators serve as critical indicators of potential complications during mechanical ventilation.
Understanding the various factors causing high-pressure alarms is crucial for healthcare providers to promptly diagnose and address issues, ensuring patient safety and optimal respiratory support.
Here are the top 5 causes of high-pressure alarm on ventilators:
- Patient Coughing or Biting on the Endotracheal Tube (ETT)
- Bronchospasm
- Secretions or Blockages
- Pulmonary Edema
- Ventilator Malfunction
[toc]
Cause 1: Secretions or Blockages
Accumulation of mucus, secretions, or blockages in the airway can severely impede the flow of air into the lungs.
When these substances build up, they create resistance within the air passages, requiring the ventilator to exert higher pressures to maintain sufficient airflow.
This increased resistance can hinder effective ventilation and oxygenation, potentially leading to respiratory distress and hypoxemia.
Additionally, patients with conditions predisposing them to excessive secretions, such as cystic fibrosis or chronic obstructive pulmonary disease (COPD), require close attention to airway clearance techniques to minimize the risk of airway obstruction and associated high-pressure alarms.
Cause 2: Patient Coughing or Biting on the Endotracheal Tube (ETT)
Coughing or biting on the endotracheal tube (ETT) can cause sudden increases in airway pressure as the patient’s respiratory efforts momentarily interfere with the ventilator’s delivery of breaths.
This can lead to transient spikes in airway pressures, triggering alarms on the ventilator.
Patient discomfort, inadequate sedation, or neurological conditions may contribute to this behavior.
Careful monitoring of the patient’s sedation level and adjustment of medication dosages to ensure adequate comfort and immobilization are crucial to prevent ETT-related complications.
Cause 3: Bronchospasm
Bronchospasm, characterized by the sudden constriction of the airway’s smooth muscles, poses a significant threat to ventilation by increasing airway resistance.
This increased resistance impedes airflow into the lungs, necessitating higher pressures to overcome the obstruction.
Common triggers of bronchospasm include allergens, respiratory infections, and exposure to irritants.
Prompt recognition of bronchospasm and initiation of appropriate bronchodilator therapy is essential to alleviate airway constriction and prevent further complications.
Cause 4: Pneumothorax
Pneumothorax, characterized by the presence of air in the pleural space surrounding the lungs, can disrupt normal lung expansion and ventilation.
As air accumulates in the pleural cavity, it compresses the lung tissue, reducing lung compliance and increasing airway pressures.
This can lead to impaired gas exchange and respiratory compromise.
Prompt recognition of pneumothorax through clinical assessment and imaging studies is crucial for timely intervention, which may include chest tube placement to evacuate air and restore negative intrathoracic pressure.
Cause 5: Pulmonary Edema
Pulmonary edema, characterized by the accumulation of fluid in the lung tissue and air spaces, poses a significant challenge to ventilation by compromising lung compliance.
As fluid accumulates within the alveoli and interstitial spaces, it impairs gas exchange and increases the work of breathing.
This can lead to elevated airway pressures as the ventilator struggles to deliver adequate tidal volumes against increased resistance.
Management of pulmonary edema involves addressing the underlying cause, such as heart failure or acute respiratory distress syndrome (ARDS), and implementing measures to optimize fluid balance and improve oxygenation.
Cause 6: Lung Compliance Changes
Conditions such as acute respiratory distress syndrome (ARDS) or pulmonary fibrosis can significantly alter lung compliance, making ventilation more challenging.
Decreased lung compliance requires higher ventilator pressures to achieve adequate tidal volumes and gas exchange.
In ARDS, for example, the loss of alveolar integrity and the development of diffuse pulmonary inflammation lead to decreased lung compliance and increased airway pressures.
Cause 7: Improper Ventilator Settings
Incorrect ventilator settings can significantly impact airway pressures and compromise patient ventilation.
Factors such as excessive tidal volume, high respiratory rate, or inappropriate inspiratory flow rates can lead to elevated airway pressures and potential lung injury.
For instance, high tidal volumes can result in barotrauma and volutrauma.
Barotrauma and volutrauma are lung injuries resulting from pressure changes and overinflation, respectively, commonly associated with mechanical ventilation.
Similarly, excessively high respiratory rates may not allow adequate time for exhalation, leading to dynamic hyperinflation and auto-PEEP.
Cause 8: Ventilator Malfunction
Mechanical issues with the ventilator, such as valve malfunction or leaks in the circuit, can disrupt the delivery of ventilation and lead to increased airway pressures.
These malfunctions may manifest as sudden spikes in airway pressures, alarms indicating circuit disconnect or discrepancies between set and delivered tidal volumes.
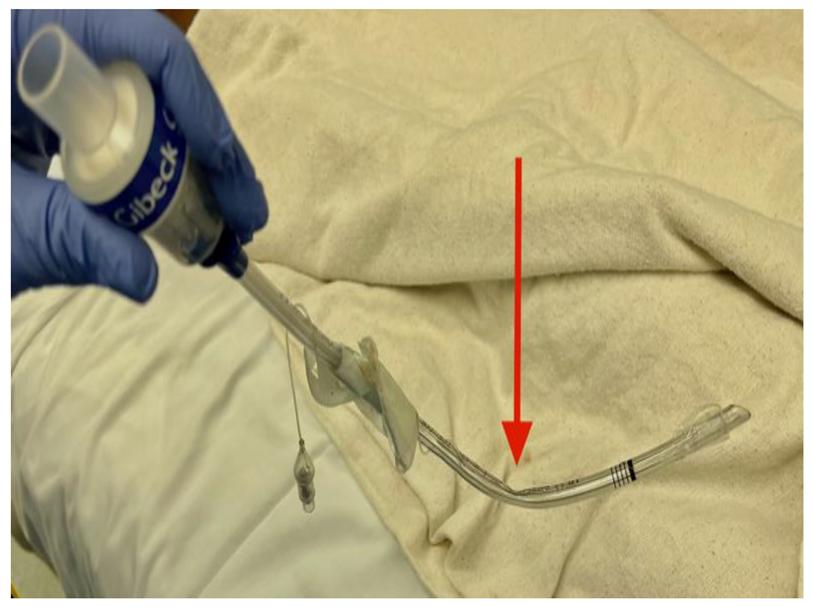
Cause 9: Endotracheal Tube (ETT)
Displacement Movement or displacement of the endotracheal tube (ETT) within the airway can compromise ventilation and lead to increased airway pressures.
Partial obstruction of the ETT due to displacement can impede airflow into the lungs, necessitating higher ventilator pressures to overcome the obstruction.
Vigilant monitoring of ETT placement, securing the tube properly, and regular assessment of lung sounds are essential to detect and prevent displacement-related complications.
Cause 10: Kinking or Compression of the Ventilator Tubing
External factors such as patient movement, positioning, or accidental compression of the ventilator tubing can disrupt airflow and increase airway pressures.
Kinking or compression of the tubing impedes the delivery of tidal volumes to the patient’s lungs, requiring higher pressures to maintain adequate ventilation.
Proper positioning of the patient and securing the ventilator tubing to prevent kinks or compression are essential measures to minimize this risk.
Cause 11: Excessive or Inadequate Sedation
The level of sedation in mechanically ventilated patients plays a critical role in maintaining respiratory stability and preventing complications such as agitation or hypoventilation.
Inadequate sedation can lead to patient discomfort, resulting in increased respiratory effort and higher airway pressures.
Conversely, excessive sedation may cause hypoventilation and hypercapnia, necessitating higher ventilator pressures to maintain adequate gas exchange.
Close monitoring of sedation levels using sedation scales and titration of sedative medications are essential to achieve optimal patient comfort and respiratory stability.
Cause 12: Excessive Chest Wall Stiffness
Conditions such as severe kyphoscoliosis or chest wall deformities can restrict chest wall movement and impair lung expansion, leading to increased airway pressures.
Reduced chest wall compliance requires higher ventilator pressures to achieve adequate tidal volumes and maintain oxygenation.
Management of chest wall stiffness involves optimizing ventilator settings to minimize work of breathing and prevent ventilator-induced lung injury.
Patient positioning maneuvers such as elevation of the head of the bed or lateral rotation may improve chest wall mechanics and facilitate ventilation.
Cause 13: Ventilator Dyssynchrony
Patient-ventilator dyssynchrony occurs when there is a mismatch between the patient’s respiratory efforts and the ventilator’s delivery of breaths.
Inadequate triggering, inappropriate flow delivery, or delayed cycling can lead to increased work breathing and elevated airway pressures.
Cause 14: Gastric Distension
Excessive insufflation of air into the stomach during positive pressure ventilation can lead to gastric distension, compromising diaphragmatic excursion, and increasing airway pressures.
Gastric distension may occur due to factors such as excessive tidal volumes, inadequate sedation, or improper ventilator settings.
Management involves minimizing gastric insufflation by optimizing ventilator settings, monitoring for signs of distension, and promoting proper ETT placement.
Suctioning of gastric contents and positioning maneuvers such as elevating the head of the bed can help alleviate gastric distension and prevent associated complications.
Collaboration with nutritionists and gastroenterologists may be necessary to develop strategies for managing gastric distension and optimizing respiratory function in mechanically ventilated patients.
High-Pressure Alarm On Ventilator Causes – FAQs
1. What does a high-pressure alarm on a ventilator mean?
A high-pressure alarm on a ventilator indicates that the pressure within the ventilator circuit or in the patient’s airway has exceeded the preset limit.
2. Which condition triggers the high-pressure alarm?
The high-pressure alarm is triggered when the pressure in the ventilator circuit or the patient’s airway exceeds the predetermined threshold set by the healthcare provider.
3. What causes high peak pressure on the ventilator?
Several factors can cause high peak pressure on the ventilator, including lung stiffness or resistance, bronchospasm, mucus plugging, improper ventilator settings, or patient ventilator asynchrony.
4. What should you do if the ventilator high-pressure alarm sounds?
When the high-pressure alarm sounds, the healthcare provider should assess the patient’s condition immediately, check for any obstructions in the airway or ventilator circuit, adjust ventilator settings if necessary, and ensure proper patient positioning.
5. How do you troubleshoot a high-pressure alarm?
To troubleshoot a high-pressure alarm, healthcare providers should first assess the patient’s condition, check for any blockages or kinks in the ventilator circuit, verify proper tube placement, evaluate lung compliance, and adjust ventilator settings as needed.
6. How do you resolve high-pressure alarms?
Resolving high-pressure alarms involves identifying and addressing the underlying cause.
This may include suctioning the airway to remove mucus, adjusting ventilator settings such as tidal volume or respiratory rate, administering bronchodilators if bronchospasm is suspected, or repositioning the patient to improve lung mechanics.
In some cases, further medical intervention or consultation with a respiratory therapist may be necessary.
7. When the high-pressure alarm on the ventilator sounds what should the nurse do?
When the high-pressure alarm on the ventilator sounds, the nurse should immediately assess the patient’s airway, check for any blockages or kinks in the ventilator circuit, ensure proper tube placement, and adjust ventilator settings as necessary to alleviate the high pressure.
8. What is the first thing you should do when you hear the ventilator alarm sounding?
The first thing to do when you hear the ventilator alarm sounding is to assess the patient’s condition and the cause of the alarm.
This involves checking the ventilator screen for alarm details, assessing the patient’s airway, and addressing any immediate concerns such as suctioning or repositioning the patient.
9. What happens in most ICU ventilators if the high-pressure limit is reached?
In most ICU ventilators, if the high-pressure limit is reached, the ventilator will activate an alarm to alert healthcare providers.
Additionally, the ventilator may temporarily pause or reduce ventilation to prevent further increases in pressure and protect the patient from potential harm.
10. What is a high respiratory rate alarm on a ventilator?
A high respiratory rate alarm on a ventilator is triggered when the patient’s spontaneous respiratory rate exceeds the preset limit programmed into the ventilator.
This alarm may indicate increased respiratory effort or agitation in the patient and may require adjustment of ventilator settings or further assessment by healthcare providers.