Diabetes is a chronic condition that affects millions of people worldwide. It not only requires careful management of blood sugar levels but also necessitates care of various body parts, especially the feet.
Diabetes can cause nerve damage and poor circulation in the feet, leading to a higher risk of complications such as infections and ulcers.
Diabetes is the leading cause of non-traumatic lower limb amputations, with foot ulcers preceding more than 80% of amputations in people with diabetes.
Let’s explore the reasons why foot care is essential for people with diabetes and find out practical tips to maintain healthy feet and prevent potential complications.
5 most common reasons for the importance of foot care in diabetes
- Prevention of Foot Ulcers
- Blood Sugar Control
- Circulation Monitoring
- Cost Saving
- Prevention of Charcot Foot
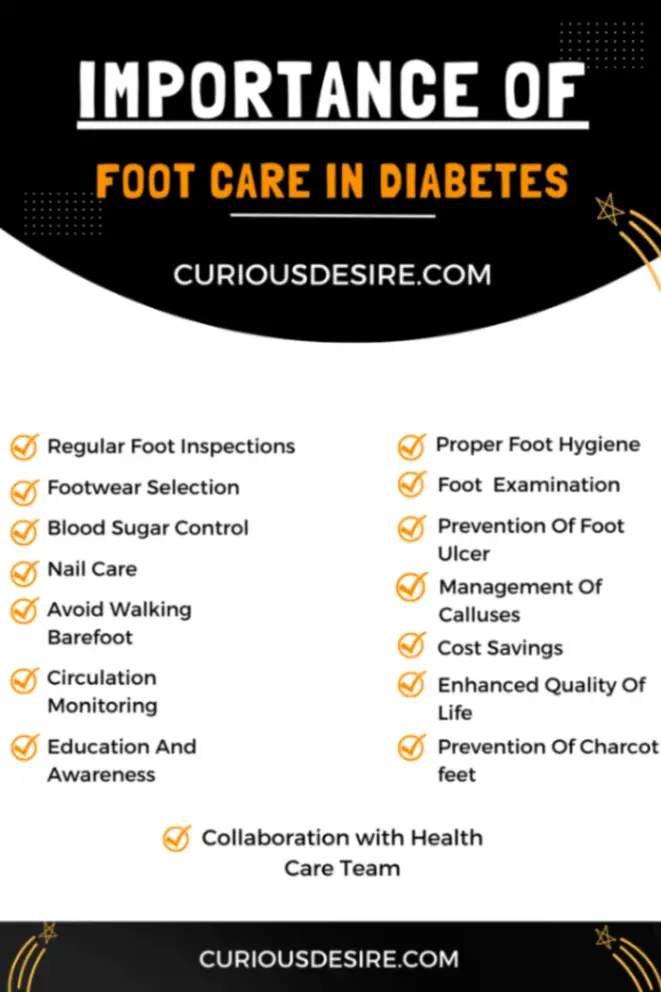
1. Regular Foot Inspections
Regularly inspect your feet for cuts, blisters, red spots, swelling, and nail problems. Use a mirror to check the soles of your feet, or ask someone for help if you cannot see them.
This is crucial for the early detection of foot issues, as diabetes can lead to nerve damage and reduced blood flow to the feet, making it harder for the body to heal injuries.
Performing a thorough foot inspection involves these steps:
- Choose the Right Time and Place: Conduct your foot inspection at the same time each day, such as before bed or after bathing, when you’re already looking at your feet.
- Inspect All Areas of Your Feet: Look at the tops and bottoms of your feet, between your toes, and at your heels. Use a mirror to view areas of your feet that are hard to see.
- Know What to Look For: You’re checking for cuts, blisters, sores, swelling, red spots, fluid discharge, nail problems, and any signs of infection. Also, look for changes in skin color, texture, and temperature differences between your feet.
- Use Your Hands: Gently feel your feet for bumps, lumps, or spots that feel unusually warm or cold, as these can indicate infection or circulation issues.
- Record your Findings: Keep a log of your inspections, noting any changes or potential issues. This record can be helpful for healthcare professionals to track your foot health over time.
2. Proper Foot Hygiene
Keeping the feet clean and dry is essential in diabetes management.
Wash your feet daily in lukewarm water. Avoid hot water, as it can cause dryness or burns. Use a mild soap to avoid skin irritation. Harsh soaps can strip the skin of its natural oils, leading to dryness.
Apply a diabetic-friendly moisturizer daily to prevent cracks in the skin, which can become entry points for infection. However, do not apply lotion between your toes, as excessive moisture in this area can lead to fungal growth.
3. Footwear Selection
Choosing proper footwear is critical for preventing foot problems in diabetes.
You should opt for comfortable, well-fitting shoes that provide adequate support and cushioning, reducing the risk of developing blisters, calluses, and other foot injuries.
Even the best-fitting shoes can become unsuitable over time as they wear out or if your feet change. Regularly assess the condition of your shoes and your feet to ensure ongoing suitability and comfort.
Replace shoes as needed, typically every 6 to 12 months for those with diabetes, depending on wear and condition.
4. Regular Foot Exams by a Healthcare Professional
Regular foot exams by a healthcare provider, such as a podiatrist, can help identify any potential issues early on
Healthcare professionals can detect problems such as changes in foot structure, nerve damage, or circulation issues and provide appropriate interventions.
This ensures that any problems are addressed promptly and appropriately.

5. Blood Sugar Control
Maintaining good control of blood sugar levels is fundamental to preventing nerve damage and circulatory issues that can lead to foot problems.
Consistently monitoring blood glucose levels and following a diabetes management plan, including medication, diet, and exercise, is vital to reducing the risk of developing foot complications.
Good blood flow is essential for wound healing and preventing infections. Activities like walking, cycling, and specific leg and foot exercises can improve circulation.
6. Prevention of Foot Ulcers
Ulcers, particularly on the feet, are a common complication of diabetes. They often result from a combination of poor circulation, foot deformities, and neuropathy.
9 to 26.1 million cases of diabetic foot ulcers are reported globally.
Maintaining optimal blood glucose levels is foundational to preventing complications of diabetes, including foot ulcers.
High blood sugar can damage nerves and blood vessels, leading to neuropathy and poor circulation, which increase the risk of foot ulcers.
Preventive measures such as regular foot inspections, proper footwear, and foot care education can significantly reduce the risk of developing ulcers.
7. Nail Care
Proper nail care is essential for diabetes, as ingrown toenails or cuts during nail trimming can lead to infections.
Trim your nails regularly to keep them at a manageable length, which reduces the risk of snagging and breaking. When trimming:
- Use a clean, sharp nail clipper or nail scissors.
- Trim nails straight across to avoid ingrown toenails.
- Avoid cutting them too short, which could expose the nail bed to infections.
- Smooth the corners with a nail file to prevent sharp edges from cutting adjacent skin.
If you notice signs of a fungal infection (discoloration, thickening, or crumbling of the nail), consult a healthcare provider for appropriate antifungal treatment.
8. Management of Calluses and Corns
The management of calluses and corns is a critical aspect of foot care for people with diabetes.
Calluses and corns are areas of thickened skin that develop as a result of excessive pressure or friction on the skin. In people with diabetes, these areas of thickened skin can lead to more serious complications, such as ulcers or infections.
Therefore, it’s essential to manage calluses and corns carefully to prevent further foot problems. You should avoid using over-the-counter callus and corn removers, as they can cause skin damage.
Healthcare professionals can provide safe and appropriate treatment for calluses and corns to prevent complications.
9. Avoid Walking Barefoot
You should avoid walking barefoot to minimize the risk of injuries, as you might not feel or notice small cuts, scrapes, or even objects on the floor due to nerve damage.
Walking barefoot can worsen existing foot conditions, such as calluses, corns, or deformities, by applying uneven pressure or causing further injury. These conditions, in turn, increase the risk of developing ulcers.
Always wear well-fitting, protective shoes or slippers, even indoors, to safeguard against injuries. Diabetic footwear is designed to reduce pressure points and provide extra support.
10. Circulation Monitoring
Monitoring blood circulation to the feet is critical if you have diabetes. Good blood flow is essential for wound healing and preventing infections.
Activities like walking, cycling, and specific leg and foot exercises can improve circulation. This active lifestyle can help in the better management of diabetes itself.
Avoiding smoking and tight footwear also promotes better blood flow.
Any signs of poor circulation, such as cold or discolored feet, should be promptly reported to a healthcare professional.
11. Cost Savings
Preventative foot care is not only a cornerstone of maintaining overall health and well-being but also a significant factor in reducing healthcare costs.
Diabetes can lead to various foot complications, including ulcers, infections, and, in severe cases, the need for amputation. These complications are often preventable with appropriate foot care and monitoring.
Preventative foot care leads to significant cost savings by avoiding expensive treatments for complications, such as hospital stays, surgeries, or long-term antibiotic therapy for infections.
12. Enhanced Quality of Life
Healthy feet are essential for mobility. Foot complications can lead to pain and discomfort, making it difficult to perform everyday activities such as walking, climbing stairs, or even standing.
By maintaining healthy feet, you can move around more freely and with less pain, leading to a more active and independent lifestyle
This active lifestyle can help in the better management of diabetes itself.
13. Education and Awareness
Providing comprehensive education on foot care to people with diabetes and their caregivers is crucial.
This includes information on the importance of foot care, signs of potential problems, and when to seek medical attention.
Understanding the potential complications and how to prevent them encourages proactive foot care and better overall diabetes management.
14. Prevention of Charcot Foot
Charcot foot is a condition that leads to the weakening of foot bones in people with significant nerve damage, potentially causing deformities.
It can develop as a result of minor injuries or stress on the foot that goes unnoticed due to the loss of sensation from neuropathy.
Effective management of diabetes and adherence to a strict foot care regimen can prevent the development of this serious complication.
15. Collaboration with the Healthcare Team
Collaboration with healthcare providers, including primary care doctors, endocrinologists, podiatrists, and other specialists, is essential for comprehensive diabetes management, including foot care.
They can offer personalized advice, professional foot care (like trimming nails and removing calluses safely), and treat any issues promptly.
Regular check-ups and communication with the healthcare team can help identify and address foot-related issues promptly.
Source: Certified foot and ankle specialist YT Channel
Conclusion
Foot care is an essential aspect of diabetes management.
Proactive foot care, including daily inspection, proper footwear, hygiene, nail care, and regular professional monitoring, is crucial for preventing complications and preserving the overall health and quality of life
Ongoing education and regular check-ups with healthcare professionals can further safeguard against complications.
Ultimately, the importance of foot care in diabetes cannot be overstated, and it remains a cornerstone of effective diabetes management and overall well-being.
Importance of Foot Care in Diabetes FAQs
1. Why is footwear important for diabetics?
When you have diabetes, you need to take extra special care of your feet. People with metabolic disease are at increased risk of suffering from impaired circulation and nerve damage in their feet
2. What is the first rule of diabetic foot care?
Inspect your feet daily. Check your feet for cuts, blisters, redness, swelling, or nail problems. Use a magnifying hand mirror to look at the bottom of your feet.
3. Are there specific exercises that can improve foot health in people with diabetes?
Exercises such as walking, swimming, and gentle stretching can improve circulation and nerve function in the feet. It’s important to consult a healthcare professional before starting any new exercise regimen.
4. What kind of footwear is important for people with diabetes?
Leather and canvas shoes are ideal because they are durable, flexible, and breathable. Avoid shoes made entirely of rubber, which can trap moisture and lead to infection. Check for a cushioned sole. Your ideal shoe should have a thick shock-absorbing sole and reduce pressure on the bottom of your foot
5. How is a diabetic foot diagnosed?
Your doctor inspects the foot, toes, and toenails for blisters, cuts, scratches, or ingrown toenails that may lead to additional ulcers. He evaluates the rate of blood flow in the foot by feeling the pulse.