Orange mucus, while unusual, can signal underlying health issues affecting the respiratory system. Understanding its causes is crucial for proper diagnosis and treatment.
In this overview, we’ll discuss the diverse factors contributing to the appearance of orange mucus, ranging from infections to environmental influences.
Let’s get into it!
Here are the top 5 causes of orange mucus:
- Environmental Factors
- Dehydration
- Infection
- Rhinitis
- Stress
[toc]

Cause 1: Infection
Infections in the respiratory tract, sinuses, or throat can trigger the production of orange mucus.
For instance, sinusitis, an inflammation of the sinus cavities often caused by a viral or bacterial infection, can lead to the accumulation of thick, discolored mucus in the nasal passages.
Similarly, bronchitis, which is characterized by inflammation of the bronchial tubes, can result in the production of orange-colored mucus due to the body’s immune response to the infection.
Pneumonia, a more serious infection affecting the lungs, can also cause mucus to become orange as the body attempts to clear the respiratory tract of pathogens.
These infections typically stimulate an inflammatory response, leading to changes in mucus consistency and coloration.
Cause 2: Environmental Factors
Other than certain infections, exposure to environmental pollutants can also irritate the respiratory tract and contribute to the development of orange mucus.
Dust, smoke, and certain chemicals present in the air can trigger inflammation of the mucous membranes lining the respiratory passages, leading to increased mucus production.
This excess mucus may take on an orange hue due to the presence of contaminants in the environment.
Individuals who live or work in environments with poor air quality, such as industrial areas or regions with high levels of pollution, may be particularly susceptible to experiencing changes in mucus coloration as a result of environmental factors.
Cause 3: Allergies
Allergic reactions to various substances, such as pollen, mold, or pet dander, can cause inflammation of the respiratory tract and the production of colored mucus, including orange.
When exposed to allergens, the body’s immune system mounts an inflammatory response, releasing histamines and other chemicals that trigger symptoms such as nasal congestion, sneezing, and excess mucus production.
The mucus produced during an allergic reaction may appear orange due to the presence of inflammatory cells and other immune system components.
Individuals with allergies may experience seasonal variations in mucus color, with symptoms worsening during periods of high allergen exposure.
Cause 4: Medication
Certain medications, particularly antibiotics or those containing iron, can alter the color of mucus.
Antibiotics are commonly prescribed to treat bacterial infections, but they can also disrupt the normal balance of bacteria in the body, leading to changes in mucus production and color.
Additionally, medications containing iron supplements may cause mucus to appear orange or darker in color.
Iron actually imparts a reddish tint to bodily fluids, including mucus, when present in high concentrations.
Cause 5: Dehydration
Dehydration can affect mucus production and consistency, leading to changes in color. When the body is dehydrated, mucus can become thicker and stickier, making it appear darker in color, including shades of orange.
Inadequate hydration can also impair the function of mucous membranes, which play a crucial role in trapping and expelling pathogens from the respiratory tract.
As a result, dehydrated individuals may be more susceptible to respiratory infections and inflammation, further contributing to changes in mucus coloration.
Maintaining proper hydration by drinking an adequate amount of fluids throughout the day is essential for supporting healthy mucus production.
According to the Mayo Clinic, men should aim for about 15.5 cups (3.7 liters) of fluids a day, while women should aim for about 11.5 cups (2.7 liters), for bodily function.
Cause 6: Diet
Dietary factors can influence the color of mucus, with certain foods and beverages containing strong pigments capable of tinting mucus orange.
For example, consuming foods rich in beta-carotene, such as carrots, sweet potatoes, or squash, can impart an orange hue to mucus due to the presence of this pigment.
Similarly, beverages like certain types of tea or those containing artificial colors may temporarily alter the color of mucus after consumption.
While the effects of dietary choices on mucus color are usually transient, individuals may notice changes in the coloration of their mucus shortly after consuming pigmented foods or beverages.
Cause 7: Bleeding
In rare cases, the presence of blood in mucus can give it an orange appearance.
This may occur as a result of nosebleeds or bleeding in the respiratory tract, which can occur due to various factors such as trauma, inflammation, or underlying medical conditions.
When blood mixes with mucus, it can produce an orange or rusty coloration, depending on the extent of bleeding and the presence of other substances in the respiratory tract.
It’s essential to seek medical attention if you notice orange-colored mucus accompanied by signs of bleeding, such as blood streaks or clots, as it may indicate a more serious underlying issue that requires evaluation and treatment.
Cause 8: Cystic Fibrosis
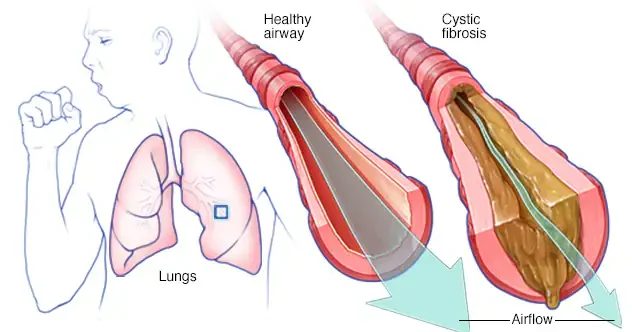
Cystic fibrosis is a genetic disorder that affects the production and consistency of mucus in the body.
In individuals with cystic fibrosis, mucus becomes thick and sticky due to a defect in the CFTR gene, leading to the buildup of mucus in the lungs and airways.
This thickened mucus can trap bacteria and other pathogens, increasing the risk of respiratory infections and inflammation.
Over time, chronic infection and inflammation can contribute to changes in mucus color, including shades of orange or yellow.
Cause 9: Chronic Obstructive Pulmonary Disease (COPD)
COPD encompasses several progressive lung diseases, including chronic bronchitis and emphysema, which can cause inflammation and mucus production in the airways.
In individuals with COPD, chronic exposure to irritants such as cigarette smoke or environmental pollutants damages the lungs, leading to the development of symptoms such as coughing, wheezing, and excessive mucus production.
The presence of colored mucus, including orange, may indicate exacerbations or worsening of COPD symptoms, often triggered by respiratory infections or environmental factors.
Management of COPD typically involves lifestyle modifications, medication, and pulmonary rehabilitation to improve respiratory function and quality of life.
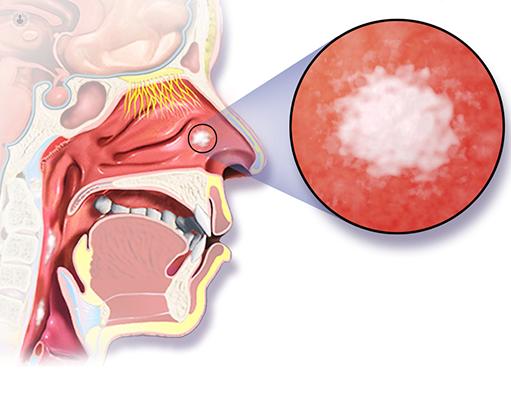
Cause 10: Rhinitis
Both allergic rhinitis (hay fever) and non-allergic rhinitis can cause inflammation of the nasal passages, leading to the production of colored mucus, including orange.
Allergic rhinitis occurs when the immune system overreacts to allergens such as pollen, mold, or pet dander, resulting in symptoms such as nasal congestion, sneezing, and excess mucus production.
Non-allergic rhinitis may be triggered by irritants such as smoke, strong odors, or changes in weather conditions, leading to similar symptoms.
The inflammation associated with rhinitis can cause changes in the consistency and color of mucus, which may vary depending on the underlying cause and individual triggers.
Cause 11: Fungal Infections
While less common than bacterial or viral infections, fungal infections in the sinuses or respiratory tract can lead to the production of orange-colored mucus.
One example is aspergillosis, a fungal infection caused by the Aspergillus species. Aspergillosis typically affects individuals with weakened immune systems or underlying lung conditions.
When the fungus invades the respiratory tract, it can cause inflammation and irritation, leading to the production of mucus with a characteristic orange or brownish tint.
Cause 12: Cancer
Certain types of cancer, such as sinus cancer or lung cancer, can cause changes in mucus color due to bleeding or other factors associated with the disease.
Sinus cancer, which affects the sinuses located in the facial bones around the nose, can cause obstruction of the nasal passages and lead to the production of blood-tinged mucus.
Similarly, lung cancer may cause bleeding within the respiratory tract, resulting in the presence of blood in mucus, which can give it an orange or reddish appearance.
Cause 13: Vitamin Deficiency
Deficiencies in certain vitamins, such as vitamin A, can affect the mucous membranes and lead to changes in mucus color.
Vitamin A plays a crucial role in maintaining the health of epithelial tissues, including those lining the respiratory tract.
Inadequate intake of vitamin A or impaired absorption can weaken mucous membranes, making them more susceptible to inflammation and infections.
As a result, changes in mucus color, including shades of orange, may occur in individuals with vitamin deficiencies.
Ensuring adequate intake of essential nutrients through a balanced diet or supplementation is important for supporting respiratory health and mucous membrane function.
Cause 14: Smoking
Smoking or exposure to secondhand smoke can irritate the respiratory tract and lead to changes in mucus color and consistency.
The chemicals present in tobacco smoke can damage the mucous membranes lining the airways, impairing their ability to produce and clear mucus effectively.
Smokers often experience chronic bronchitis, characterized by persistent coughing and mucus production, which may result in the presence of colored mucus, including orange or brownish tint.
Quitting smoking and avoiding exposure to secondhand smoke are essential steps for improving respiratory health and reducing the risk of associated complications.
Cause 15: Stress
Prolonged periods of stress can weaken the immune system and increase susceptibility to infections, which may manifest as changes in mucus color.
Stress hormones such as cortisol can suppress immune function, making individuals more vulnerable to respiratory infections and inflammation.
Chronic stress can also exacerbate existing respiratory conditions, leading to an increase in mucus production and changes in its coloration.
Additionally, stress can contribute to unhealthy coping behaviors such as smoking or poor dietary choices, further impacting respiratory health.
Managing stress through relaxation techniques, exercise, and social support can help support immune function and reduce the risk of respiratory issues associated with stress.
Orange Mucus Causes FAQs
1. What causes orange mucus?
Orange mucus can be caused by various factors, including infections such as sinusitis or bronchitis, exposure to environmental pollutants, allergies, medication side effects, dehydration, dietary factors, bleeding in the respiratory tract, certain medical conditions like cystic fibrosis, or chronic obstructive pulmonary disease (COPD).
2. What Colour is unhealthy mucus?
Unhealthy mucus can vary in color depending on the underlying cause. In general, mucus that is green, yellow, or brown may indicate an infection, while clear or white mucus is typically considered normal.
Red or pink-tinged mucus may indicate the presence of blood and should be evaluated by a healthcare professional.
3. What causes mucus problems?
Mucus problems can be caused by a variety of factors, including infections (bacterial, viral, or fungal), allergies, environmental irritants, smoking, dehydration, certain medications, autoimmune conditions, structural abnormalities in the respiratory tract, or chronic respiratory conditions such as asthma or chronic obstructive pulmonary disease (COPD).
4. What color is allergic rhinitis mucus?
In allergic rhinitis, mucus is typically clear or white. However, during an allergic reaction, mucus production may increase, leading to nasal congestion, runny nose, and post-nasal drip.
In some cases, allergic rhinitis may cause clear or white mucus to become thicker or discolored due to secondary infections.
5. Does mucus color matter?
Yes, mucus color can provide clues about underlying health conditions. While clear or white mucus is generally considered normal, changes in color, such as green, yellow, or orange, may indicate the presence of infection or inflammation.
Red or pink-tinged mucus may indicate bleeding. However, mucus color alone is not always a reliable indicator of illness, and other symptoms should be considered as well.
6. What are the 3 symptoms of rhinitis?
The three primary symptoms of rhinitis are nasal congestion, runny nose (rhinorrhea), and sneezing.
Other common symptoms may include itching of the nose, eyes, or throat; post-nasal drip; coughing; watery eyes; and reduced sense of smell or taste.
7. What organ does rhinitis affect?
Rhinitis primarily affects the nasal passages, which are responsible for filtering, warming, and humidifying air before it reaches the lungs.
However, rhinitis can also affect other areas of the respiratory system, such as the sinuses, throat, and ears.
8. How to relieve rhinitis?
Relief for rhinitis symptoms may include using over-the-counter or prescription antihistamines, nasal decongestants, nasal corticosteroids, saline nasal sprays, or allergy medications.
Avoiding triggers such as allergens or irritants, using air purifiers, practicing good hygiene, and staying hydrated may also help alleviate symptoms.
9. Is rhinitis serious?
In most cases, rhinitis is not considered serious and can be managed with proper treatment and lifestyle modifications.
However, severe or chronic rhinitis may significantly impact quality of life and may be associated with complications such as sinus infections, ear infections, or sleep disturbances.
10. How can I permanently cure allergic rhinitis at home?
While allergic rhinitis cannot be permanently cured, it can be effectively managed with proper treatment and lifestyle modifications.
Home remedies for allergic rhinitis may include avoiding triggers, using air purifiers, practicing nasal irrigation with saline solutions, maintaining good indoor air quality, and incorporating anti-inflammatory foods into the diet.
11. What is the best medicine for allergic rhinitis?
The best medicine for allergic rhinitis depends on the severity of symptoms and individual response to treatment.
Common medications for allergic rhinitis include antihistamines (both oral and nasal), nasal corticosteroids, decongestants, leukotriene receptor antagonists, and allergy shots (immunotherapy).
12. What are the 4 stages of rhinitis?
The four stages of rhinitis include the prodromal stage (initial symptoms such as itching or sneezing), the early stage (nasal congestion and runny nose), the peak stage (severe symptoms), and the late stage (symptoms may decrease or worsen depending on treatment and environmental factors).
13. Does allergic rhinitis have mucus?
Yes, allergic rhinitis can cause increased mucus production, leading to symptoms such as nasal congestion, runny nose (rhinorrhea), and post-nasal drip.
However, the mucus associated with allergic rhinitis is typically clear or white unless a secondary infection develops.
14. What color is nasal drainage with rhinitis?
Nasal drainage with rhinitis may vary in color depending on the underlying cause. In allergic rhinitis, nasal drainage is typically clear or white.
However, if rhinitis is complicated by a bacterial or viral infection, nasal drainage may become discolored, such as green, yellow, or orange.
15. What does nasal mucosa look like in allergic rhinitis?
In allergic rhinitis, the nasal mucosa may appear swollen, pale, or bluish-gray in color due to inflammation and congestion.
Additionally, the nasal passages may be filled with clear or white mucus, and the nasal turbinates (structures inside the nose) may be enlarged or congested.
16. How do I know if my rhinitis is allergic?
Allergic rhinitis is characterized by symptoms such as nasal congestion, runny nose, sneezing, itching of the nose, eyes, or throat, and symptoms that occur seasonally or upon exposure to specific allergens.
Diagnosis of allergic rhinitis may involve allergy testing, medical history evaluation, and physical examination by a healthcare professional.